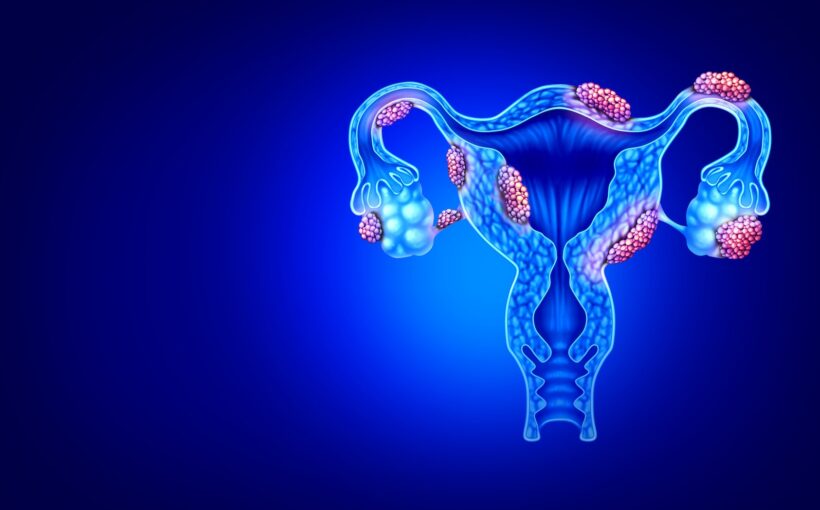
Endometriosis is a debilitating condition which affects 10% of women worldwide. The condition can have a serious affect on a person’s quality of life, often causing a range of symptoms including chronic pain, fatigue and pain during sex.
Despite how common endometriosis is, most women wait on average 7.5 years for a diagnosis in the UK. Not only does this mean many years without treatment, it also puts them at risk of even greater health problems. Untreated endometriosis can lead to organ damage (including the uterus and bowels) and infertility.
There’s currently no cure for endometriosis. This may be due to how complex endometriosis is, affecting many different parts of the body – meaning researchers still don’t fully understand all the causes of the disease.
In the last few years, studies have found that the immune system is also affected by endometriosis. It’s still unclear whether the immune system causes endometriosis or is merely affected by it. But exploring this link could eventually lead to better targeted treatment for the condition.
Inflammation and immunity
To understand how our immune system and endometriosis are connected, it’s first important to understand an immune system process called inflammation.
Inflammation is a key feature of how our immune system works. When the body encounters a harmful pathogen (such as a virus or bacteria), our immune system is triggered. The body then secretes special proteins called cytokines, which tell our immune cells what to do.
The symptoms you experience as a result of inflammation will depend on the reason these cells have been mobilised. For example, if your inflammation is caused by a cut to your finger, you may find the area around the cut becomes hot, red and swollen as the immune system works to combat pathogens and repair the damage. If inflammation is caused by a virus, you might experience flu-like symptoms – such as a fever.
For the most part, inflammation is a short-term process. But sometimes the immune system gets things wrong, and your body continues to send inflammatory cells and cytokines even when there’s no threat. Autoimmune diseases such as rheumatoid arthritis are an example of this, where the body’s immune system continues to attack, leading to long-term inflammation in the joints.
Inflammation is also a normal feature of the menstrual cycle.
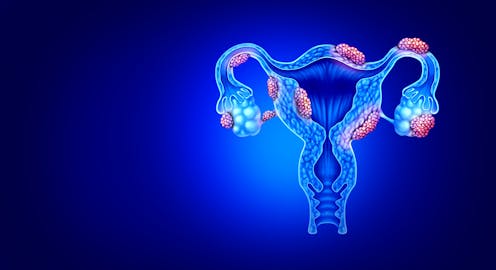
The normal menstrual cycle consists of two phases: the follicular phase (from the first day of the period until ovulation) and the luteal phase (from ovulation until your period starts). Most inflammation during the menstrual cycle happens in the uterus, but changes may also occur throughout the body.
During the follicular phase, there are increased levels of oestrogen circulating in the body. Oestrogen stimulates the lining of the uterus to thicken in preparation for a fertilised embryo.
But some immune cells have specific receptors which recognise oestrogen, causing them to initiate an immune response. This readies the body to fight off any foreign invaders so it’s healthy for pregnancy, should fertilisation occur. As such, women will be less susceptible to infections during the follicular phase. However, women with autoimmune diseases may experience more symptoms at this stage.
But in order not to reject a fertilised egg, the immune system is then suppressed during the luteal phase – which may subsequently increase risk of infection, and cause relief from some autoimmune symptoms.
Endometriosis and immunity
Research has observed multiple immune system changes in people with endometriosis.
One study found patients with endometriosis had elevated inflammation levels (specifically higher levels of cytokines). Research has also shown that people with endometriosis have disturbed immune cell function – namely a specific type of immune cell called natural killer cells.
These have a vital role in fighting viruses and tumours, but research shows they function more poorly in people with endometriosis. The uterine lining in patients with endometriosis is also shown to produce excess molecules called chemokines that attract other immune cells, worsening inflammation.
Again, it’s still not certain whether altered immune function causes endometriosis or is merely a symptom of the disease. But immune system dysfunction may explain why there’s a suspected association between people with endometriosis and autoimmune disorders such as lupus, rheumatoid arthritis and inflammatory bowel disease.
Elevated inflammation levels also mean that women with endometriosis may be more likely to experience worse symptoms during infections. For example, research has found that when patients with endometriosis catch COVID-19, their symptoms appear to be worse than people who don’t have the condition.
COVID-19 may also worsen endometriosis symptoms – particularly pelvic pain, depression, fatigue and gastrointestinal issues. A recent study has also found that women with endometriosis were 22% more likely to suffer long COVID – and their long COVID symptoms may last longer.
While it’s currently not known how precisely the immune system is linked with endometriosis (and whether it causes the disease), working to further understand this relationship could be key in helping develop better treatments – or possibly even a cure – for endometriosis.
Research into this disease is still severely under-funded, and the time to diagnosis is far beyond what would be expected from other chronic conditions – such as asthma or diabetes. It’s clear that greater priority needs to be placed into researching endometriosis and its causes to help provide new insights and better treatment for the millions of women affected.
![]()
April Rees does not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and has disclosed no relevant affiliations beyond their academic appointment.