
Since the world’s first human baby was born by in vitro fertilisation (IVF) in the UK in 1978, over 10 million IVF babies have been born globally. Assisted reproductive technologies (ART) have also become even more sophisticated, now including egg-freezing and intracytoplasmic sperm injection (ICSI).
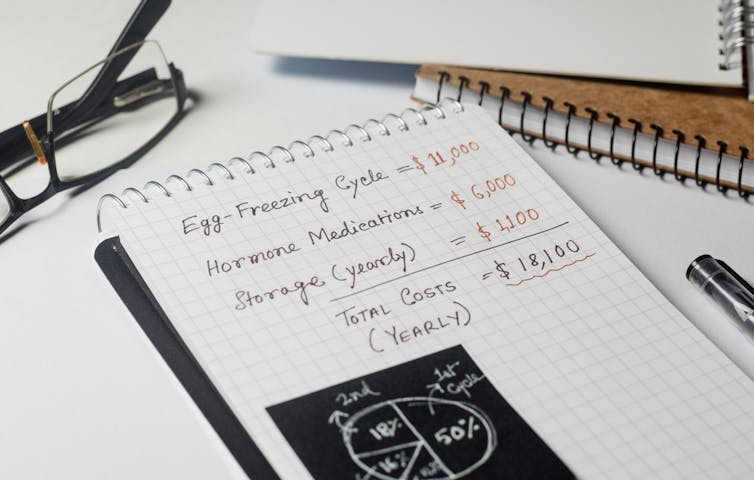
But alongside these new fertility possibilities, the technology has also brought challenges. Access to publicly funded fertility treatment is not universal, and success rates are limited. This means many people globally are forced to pay privately – if they can afford it – often for multiple cycles of treatment. This can equate to tens of thousands of pounds.
For some, it might also mean travel overseas. Inequalities in access and care in the UK have been linked to factors such as patient sexual orientation, ethnicity, age and weight.
Infertility is a disease of the reproductive system affecting one in six people, or around 17.5% of the global adult population, according to the World Health Organization.
This article is part of Women’s Health Matters, a series about the health and wellbeing of women and girls around the world. From menopause to miscarriage, pleasure to pain the articles in this series will delve into the full spectrum of women’s health issues to provide valuable information, insights and resources for women of all ages.
As well as medical issues, sexual orientation or lack of a partner can affect the ability to conceive. But despite its prevalence among the working age population, and the considerable psychological and social tolls it can bring, discussion of infertility has historically been silenced in public discourse and in the workplace.
Until recently, employers’ attention to reproductive journeys has been limited to mainly maternity provisions. This has been mandated by employment legislation in many countries for some time.
But changing social attitudes, advances in technology and business pressures have increased the attention being paid to fertility treatment by many employers in the developed world. This is often driven by business logic: supporting staff through IVF and the like will help with recruitment, performance, retention and engagement.
Supporting different fertility journeys
Indeed, employer interest in fertility treatment appears to have originated in Silicon Valley in the US. Apple and Facebook introduced fertility benefits (paid IVF and egg freezing) in 2014 as a weapon in the “war for talent”. This was controverisal, however, with companies accused of essentially trying to bribe women into delayed childbearing.
In the UK, the focus is generally on wellbeing. Workplace benefits often centre on fertility policies and time off, flexibility and workplace adjustments. But only 3% of employers said they offer such provisions to a significant extent in a 2022 survey. This puts fertility, alongside menstruation, bottom of the list of wellbeing supports aimed at certain employee groups.
Arguably, the emergence of employer interest in assisted fertility technology has furthered “reproductive stratification”. Research on this issue defines this as when “some categories of people are empowered to nurture and reproduce, while others are disempowered”
Among the minority of employers that offer fertility-related policies and support, it tends to be aimed at permanent, highly valued staff in countries in the global north such as the US, UK and Japan. And so, large proportions of the world’s workforce are missing out.
Migrants and workers in precarious employment also miss out on other things that help with reproductive journeys. This can include job security, protection from dismissal, decent wages, access to sick leave, access to maternity and paternity provisions, and well-trained and supported line managers.
When policies are in place, they are not always inclusive of all employees and all fertility journeys. Our research shows policies often neglect partners and non-normative families (same-sex couples and those pursuing motherhood alone). They often focus on a set number of days off for treatment cycle(s). This may not be sufficient and also fails to consider the needs of staff where treatment is unsuccessful.
And even when employees can access fertility treatments via progressive employment provisions, they often end up being penalised via discrimination or negative career consequences. We found this during a study in which participants reported having to go part-time, switch career focus, leave jobs, or were just generally disadvantaged at work after embarking on a fertility journey.
Similar findings have been reported in international studies and surveys by campaign groups such as Fertility Matters at Work and Pregnant then Screwed. Since women are most likely to experience these negative career consequences, this means increased take-up of fertility treatment could further existing gendered inequalities in the workplace.
A more equitable future
To fully optimise the hope created by ARTs, governments around the world should expand publicly funded provisions as much as possible (bearing in mind other healthcare commitments) and ensure equitable access and care. Employment legislation should also protect workers from discrimination on the grounds of accessing ARTs and allow suitable time off.
There is some hope. The UK parliament is currently considering a private members’ bill to allow people to take time off work for appointments and treatment, but unfortunately it hasn’t made much progress to date.
A few other countries have already taken action, however. Malta legislates for 100 hours’ paid IVF leave (per cycle, up to three cycles) split between the “receiving person” and their partner. Korea provides three days’ leave per year (one paid) and protection from discrimination. Japan has also introduced provisions for public workers.
Other recent UK developments include workplace guides from professional body The Chartered Institute of Personnel and Development (CIPD) and government funding for charities to develop resources aimed at small and medium-sized enterprises (SMEs). These are welcome.
But until the government can step up to provide universal cover, organisations should not think of fertility benefits strictly in terms of a cost-benefit calculation. Employers must take a compassionate and fully inclusive approach to supporting their employees’ fertility journeys.
Krystal was PI on an empirical research project connected to this article, which was funded by The Leverhulme Trust (Research Project Grant) Krystal is a member of advisory boards for the charities Working Families and Tommy’s. She has also contributed to resources (book chapters, surveys and guides) for the CIPD and is a CIPD member
Clare Mumford and Michael Carroll do not work for, consult, own shares in or receive funding from any company or organisation that would benefit from this article, and have disclosed no relevant affiliations beyond their academic appointment.



